Examples of Home Health Care Quality Measures for Consumers Agency for Healthcare Research and Quality
Table of Content
- What Parents Have to Say: Content and Actionability of Narrative Comments from Child HCAHPS Survey
- Evaluate & CompareHealth Care Facilities
- Events
- Adjusting for Patient Characteristics to Compare Quality of Care Provided by Serious Illness Programs
- Contacts for the quality indicators for in-home aged care project
- HHS Guidance Repository
- Measure KPIs And Grow Your Home Health Business With Timeero
This study was a cross-sectional mixed-methods analysis of in-depth multimodal data from 31 POs affiliated with 22 purposefully selected health systems in 4 states. This study offers a provisional framework that can help in structuring thinking, policy and practice. By outlining the range of domains relevant to remote antenatal care, this framework is likely to be of value in guiding policy, practice and research. The objective of this paper is to review evidence on survey administration strategies to improve response rates and representativeness of patient surveys. Exploring how often inquiries turn into admissions will help you answer various questions.

At the same time, your team will understand that KPIs hold them accountable for meeting their performance goals. The only way agencies can confirm that their business objectives are being fulfilled is by tracking and measuring their performance. Tightening budgets and keeping up with ever-evolving regulations, policies, and processes in this dynamic industry have put a lot of pressure on home health care agencies. The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. The RAND Corporation is a research organization that develops solutions to public policy challenges to help make communities throughout the world safer and more secure, healthier and more prosperous. This issue brief describes challenges and opportunities related to measuring, reporting, and monitoring the quality of HCBS sponsored by Medi-Cal.
What Parents Have to Say: Content and Actionability of Narrative Comments from Child HCAHPS Survey
We would, in effect, be carrying out a targeted and focused sampling of the care provided. So rather than developing long lists of indicators to assess every aspect of care, we should ask how many indicators are needed to make a reasonable assessment of a specific underlying construct. If the indicator set covers multiple constructs , then we should look for redundancy within rather than across these domains, as we still need content validity for each of these constructs. The purpose, broadly speaking, of all indicators is to monitor and hopefully improve the quality and value of care provided in the health system.
To calculate it, divide the number of clients admitted by the total number of people who made an inquiry about your services in the same period. If the client turnover is significant, it might imply poor client satisfaction and the low quality of the service provided. You can calculate it by dividing the number of all active clients during a time period by the number of months care was provided.
Evaluate & CompareHealth Care Facilities
The Centers for Medicare & Medicaid's Services reports many of the NQF-endorsed measures on its Home Health Compare website. Some other report developers also present this data, sometimes along with other information about home health care. For a list of home health outcome measures, please refer to the Home Health Outcome Measures Table, which can be located via the link for Home Health Measures Tables in theDownloadssection below. Technical Specifications for calculating OASIS-based outcome measures, patient-related characteristics measures, and the factors used to risk adjust outcome measures, can be accessed via the link for Technical Documentation of OASIS-Based Measures in theDownloadssection below.
The objective was to conduct a systematic review of toolkit evaluations intended to spread interventions to improve healthcare quality. We aimed to determine the components, uptake, and effectiveness of publicly available toolkits. Besides financial profit drivers, such as price or service volume, non-financial profit drivers are also significant to consider. They include customer satisfaction, productivity, service quality, employee satisfaction, etc. Some of these drivers are mentioned above and below, as key performance indicators for home health care.
Events
On the other hand, annual revenue is significant for determining whether you are paying yourself and your staff properly. Most organizations set objectives, and KPIs are used to show the direction an organization is moving into by providing objective and comparable data, expressed by numbers. Variations in quality of Home Care between sites across Europe, as measured by Home Care Quality Indicators. Quality of care in European home care programs using the second generation interRAI Home Care Quality Indicators . HHS is committed to making its websites and documents accessible to the widest possible audience, including individuals with disabilities.
That’s why tracking key performance indicators for home health care has become critical, enabling agencies to have a clear insight into their business performance and improve it. Potentially avoidable events serve as markers for potential problems in care because of their negative nature and relatively low frequency. The potentially avoidable events reported are outcome measures, in the sense that they represent a change in health status between start or resumption of care and discharge or transfer to inpatient facility. All the potentially avoidable event measures are adjusted for variation in patient characteristics.
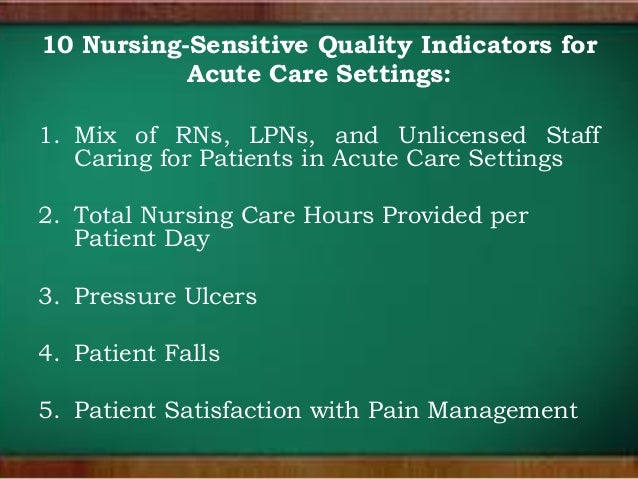
The consortium identified, assessed, and consulted on evidence-based quality indicators across five quality of care domains and examined the use of consumer experience and quality of life assessment tools. While individual quality indicators have been extensively studied, and much written about the criteria for a good indicator, considerably less attention has been devoted to the criteria and desirable characteristics of sets of indicators. The paper by Xu and colleagues shows that there is much to be gained by shifting the level of analysis to reflect on the underlying constructs and wider purpose of indicator sets. Rather than accumulating and aggregating multiple individual indicators, in the hope that they will meet the needs of users and health systems, we could endeavour to define the fundamental purpose of indicator sets and then choose relevant component indicators. In this editorial, we attempt to define a core set of questions that could help to shape and refine the core features of an indicator set. NJ DOH uses research tools or modules developed by the Agency for Healthcare Research and Quality to measure different aspects of quality of care in hospitals.
Yet, any monitoring activity has a cost, both visible in the form of resources consumed in producing them and, largely invisible, in terms of staff time consumed in recording and submitting the information, unless it can be derived directly from electronic health records. The principle, for instance, of consuming no more than 1% of a provider organisation’s budget on indicator collection might do a great deal to focus indicator sets on issues that are of real value to multiple stakeholders. Patients and their families may use publicly available quality indicators to inform their choice for a particular provider, but will also rely on other sources that they may well regard as more important than formal indicators. Providers may use quality indicators internally to monitor safety and to support their efforts to improve care; they may also benchmark their care in relation to similar institutions. All these users want to measure the quality of care, but each group faces different challenges and poses different questions.
Technical documentation for calculating process measures can be accessed via the link to Technical Documentation of OASIS-Based Measures in theDownloadssection below. New Jersey is home to over 2,000 licensed hospitals, nursing homes, and medical care facilities. The New Jersey Department of Health works to ensure that citizens receive appropriate levels of care in every regulated facility.
Changes cannot of course be too frequent; otherwise, the adjustments to the set will become burdensome and tracking change over time will become more difficult. The relationships between these different constructs must also be considered; for instance, care may be efficient, but not equitable, or conversely equitable but not efficient. In practice, however, most organisations simply produce long lists of specific indicators with no indication of what construct these intend to measure, or whether the set is valid to coherently measure that construct. However, this process will also greatly clarify the construct and ensure that each individual indicator does contribute to the overall measurement objective. Most HH QRP measures are assessment-based measures created using the OASIS assessment tool data. OASIS-based measures are created using counts of HH quality episodes and can be either process our outcomes measures.
OASIS-based process measures are not risk-adjusted show how often home health agencies gave recommended care or treatments that research shows get the best results for most patients. OASIS-based outcome measures are risk adjusted using available OASIS-based data elements. The assumption of most organisations developing and requiring indicators seems to be that the best way to ensure overall quality of care is to measure every possible aspect of care provided. An alternative approach would be to focus on specific underlying constructs of interest for a particular purpose, such as the safety or equity of care provided, and identify a set of indicators that would reliably and validly assess that construct.
The data collected by tracking KPIs provides statistics and enables a home healthcare agency to analyze its progress over a specific time, compare it to its industry peers and look for ways to improve its performance. The National Quality Forum , a multistakeholder organization established to standardize health care quality measurement and reporting, has endorsed several consensus standards for skilled home health services. Process measures evaluate the rate of home health agency use of specific evidence-based processes of care. The HH process measures focus on high-risk, high-volume, problem-prone areas for home health care. These include measures pertaining to all or most home care patients, such as timeliness of home care admission.
Key performance indicators are quantifiable or measurable values that reveal whether an organization is accomplishing its goals. Percentage of patients needing emergent care for wound infections or deteriorating wound status. Technical documentation for calculating potentially avoidable event measures can be accessed via the link to Technical Documentation of OASIS-Based Measures in theDownloadssection below. TheDownloadssection also has a link for the Outcome-Based Quality Monitoring Manual which contains additional information about the PAE measures. For a list of the potentially avoidable event measures, please refer to the Home Health PAE Measures Table, which can be located via the link to the Home Health Measures Tables in theDownloadssection below. If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service.
Despite efforts by insurance companies and other payers to move toward compensating physicians based on the quality and value of care they provide, most physicians employed in group practices owned by health systems are paid primarily based on the volume of care they provide. Drawing upon decades of experience, RAND provides research services, systematic analysis, and innovative thinking to a global clientele that includes government agencies, foundations, and private-sector firms. Over time, it may indicate whether your agency is understaffed, leading your caregivers to burnout and reducing the quality of service, or overstaffed, causing too high overhead expenses. Calculate this KPI by dividing the number of clients that stopped services during a specific period by the total number of clients with the agency during the same time period.
Comments
Post a Comment