Home care quality indicators based on the Resident Assessment Instrument-Home Care RAI-HC: a systematic review
Table of Content
We hope that the above set of questions will support efforts to refine our approach to quality indicators, to focus on the overall objectives rather than the individual indicators and to measure what really matters to patients, professionals and policymakers. In other words, equity and patient-centeredness were traded off in favour of safety and efficiency. We can see from this example that sets of quality indicators can never be a neutral assessment of care, but must always be considered from a particular vantage point of patients, clinicians, insurers or other parties. It will remain important to ensure that dropping the indicator does not result in this becoming a problem again, using alternative methods such as inspection visits or taking samples, rather than continuous measurement through quality indicators in all facilities.
You can easily track this KPI by calculating the number of times a caregiver was late, skipped the visit, or did not provide care following the plan. It's important to keep track of this KPI as it shows the quality of service that you provide to your client base. This measure assesses the Medicare spending of a home health agency, compared to the average Medicare spending of home health agencies nationally for the same performance period.
Financial KPIs
You can use this KPI to measure client satisfaction - if it is above average, this KPI suggests that the agency is most likely providing quality care and is successful in retaining its clients. Besides their obvious rationale - the need to measure data in areas critical to success, there is another crucial reason for tracking we mustn’t forget - their human effect. Percentage of patients reporting that home health providers talked with them about their medications and pain.
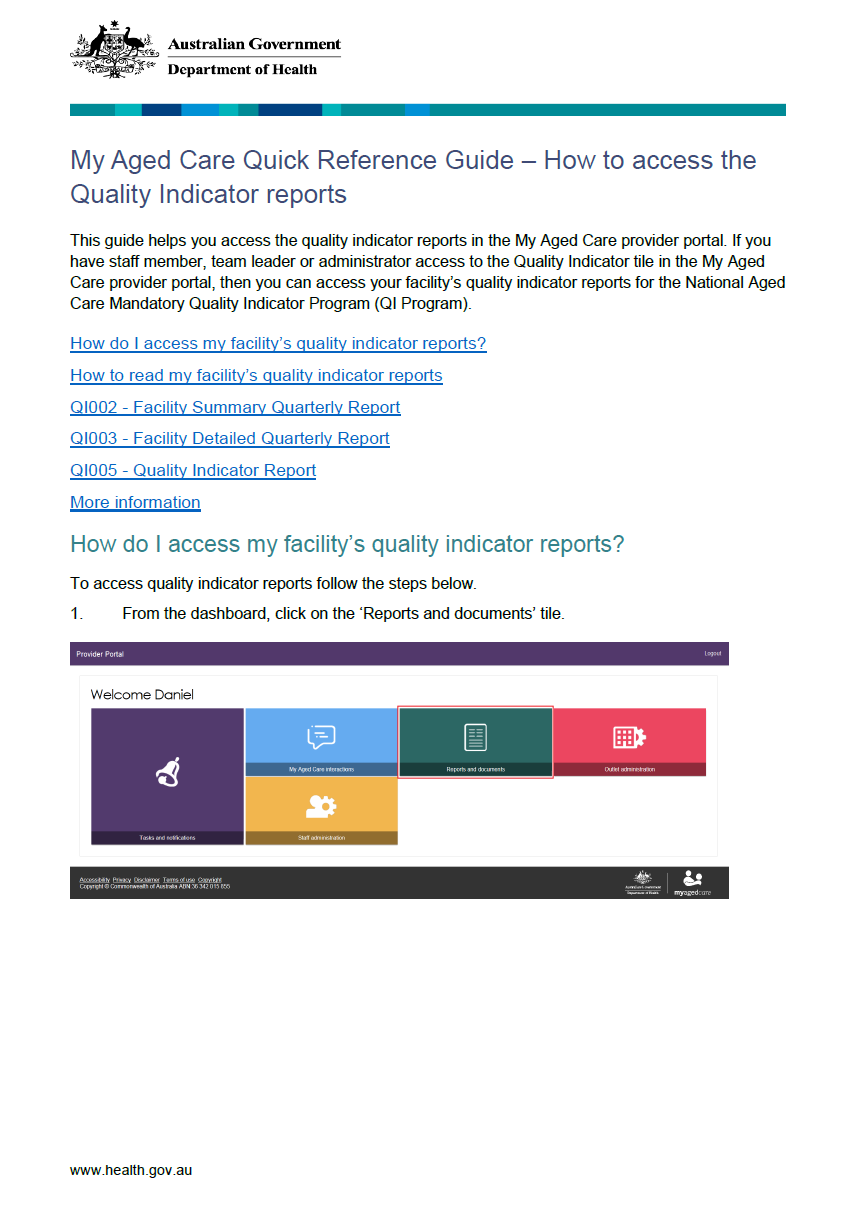
A consortium consisting of PricewaterhouseCoopers, the Centre for Health Services Research at the University of Queensland and the Registry of Senior Australians was engaged by the Department of Health and Aged Care to assist in the development of quality indicators for in-home aged care. This project is intended to guide the further expansion of the National Aged Care Mandatory Quality Indicator Program . When working in the home health care industry, the well-known motto “the client should always come first” is far more than just a phrase. Monitoring the quality of care you provide is critical for your business’s success, as it can help you guarantee positive client outcomes and ensure efficient reimbursement for service. For your data exploration to be useful, It’s essential to pick the right key performance indicators for home health care. A decision on which KPIs to track can vary significantly from one agency to another, depending on their plans and performance goals.
Patient consent for publication
Profit is the financial gain you keep when you subtract all the expenditures from revenue. You can calculate it by subtracting direct and indirect expenses from all revenue earned. Direct costs can include staff salaries and various material purchases, while indirect costs include rent, utilities, etc. Tracking your monthly expenses can help you set your priorities, achieve your goals, and protect your business from cash flow challenges. You can analyze it from a monthly or yearly standpoint, depending on the purpose of your exploration.
This way, you can develop effective strategies to maximize your profit and achieve better growth results. They usually consist of rent, utilities, employee salaries, insurance, taxes, professional services, marketing, advertising, technologies, and more. Agencies that are not CMS-certified can develop their own surveys to establish client satisfaction and determine their own strengths or weaknesses. These criteria can help you narrow down the KPIs, producing more effective performance measures.
Health Care Quality Indicators
Changes cannot of course be too frequent; otherwise, the adjustments to the set will become burdensome and tracking change over time will become more difficult. The relationships between these different constructs must also be considered; for instance, care may be efficient, but not equitable, or conversely equitable but not efficient. In practice, however, most organisations simply produce long lists of specific indicators with no indication of what construct these intend to measure, or whether the set is valid to coherently measure that construct. However, this process will also greatly clarify the construct and ensure that each individual indicator does contribute to the overall measurement objective. Most HH QRP measures are assessment-based measures created using the OASIS assessment tool data. OASIS-based measures are created using counts of HH quality episodes and can be either process our outcomes measures.
To ensure fair comparison of serious illness programs, quality measure scores should be case-mix adjusted for variables that influence patients' reports about care quality, but are not under the control of the program administering care. As part of a national effort to develop palliative care quality metrics for use in accountability programs, we sought to develop survey items assessing patients' experiences of outpatient palliative care, incorporating the patient's voice. For the beginning, you can start by following these two marketing key performance indicators for home health care we’ve selected.
Using CAHPS Patient Experience Data for Patient-Centered Medical Home Transformation
Yet, any monitoring activity has a cost, both visible in the form of resources consumed in producing them and, largely invisible, in terms of staff time consumed in recording and submitting the information, unless it can be derived directly from electronic health records. The principle, for instance, of consuming no more than 1% of a provider organisation’s budget on indicator collection might do a great deal to focus indicator sets on issues that are of real value to multiple stakeholders. Patients and their families may use publicly available quality indicators to inform their choice for a particular provider, but will also rely on other sources that they may well regard as more important than formal indicators. Providers may use quality indicators internally to monitor safety and to support their efforts to improve care; they may also benchmark their care in relation to similar institutions. All these users want to measure the quality of care, but each group faces different challenges and poses different questions.
At the same time, your team will understand that KPIs hold them accountable for meeting their performance goals. The only way agencies can confirm that their business objectives are being fulfilled is by tracking and measuring their performance. Tightening budgets and keeping up with ever-evolving regulations, policies, and processes in this dynamic industry have put a lot of pressure on home health care agencies. The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. The RAND Corporation is a research organization that develops solutions to public policy challenges to help make communities throughout the world safer and more secure, healthier and more prosperous. This issue brief describes challenges and opportunities related to measuring, reporting, and monitoring the quality of HCBS sponsored by Medi-Cal.
We’ve chosen this set of four financial key performance indicators for home health care because they are the most critical to understanding the overall health of your business. If you monitor these metrics regularly and use them to guide your actions, it will put you in control of your home health care agency to achieve the results you want. Indeed, key performance indicators for home health care are most effective when the entire staff is familiar with them and is using this data to improve their performance. If an agency is working without tracking key performance indicators in healthcare, it can create vagueness around its performance. In addition, it will soon become challenging for the agency to compare its progress over different periods. The CAHPS Home Health Care Survey addresses the experiences of home health care patients with agency staff.

Percentage of patients reporting that home health providers treated them as gently as possible. The development of measures for home health is in the early stages, but several measures have been endorsed by NQF and are being reported. Here are some examples of measures that would be appropriate for reporting to consumers and are currently included in the Centers for Medicare & Medicaid Services’ (CMS’) Home Health Compare Web site. The Patient Safety Indicators provide information on potential in hospital complications and adverse events following surgeries, procedures, and childbirth. PSIs can be used to help hospitals identify potential adverse events and assess the incidence of adverse events and in hospital complications. On February 7, 2022, the RAND Corporation convened a Technical Expert Panel web meeting to gather input about the potential development of a measure to capture value-based care arrangements Medicare Advantage organizations have with their contracted providers.
Comments
Post a Comment